Media Release: Nelson, New Zealand – 10 July 2024 – Kimer Med $10M closer to…
Vaccines are only part of the solution to the significant harm caused by viral disease. Here’s why.
There’s been a huge amount of interest in and discussion about vaccines over the past couple of years, and more than 66% of the world’s population has now received at least one dose of a Covid-19 vaccine1. Vaccines are designed to pre-arm your immune system to recognise and defend the body against a particular virus, and therefore need to be administered before you are infected. Generally, vaccines don’t produce an effect immediately and there is some delay while your immune system develops its response.
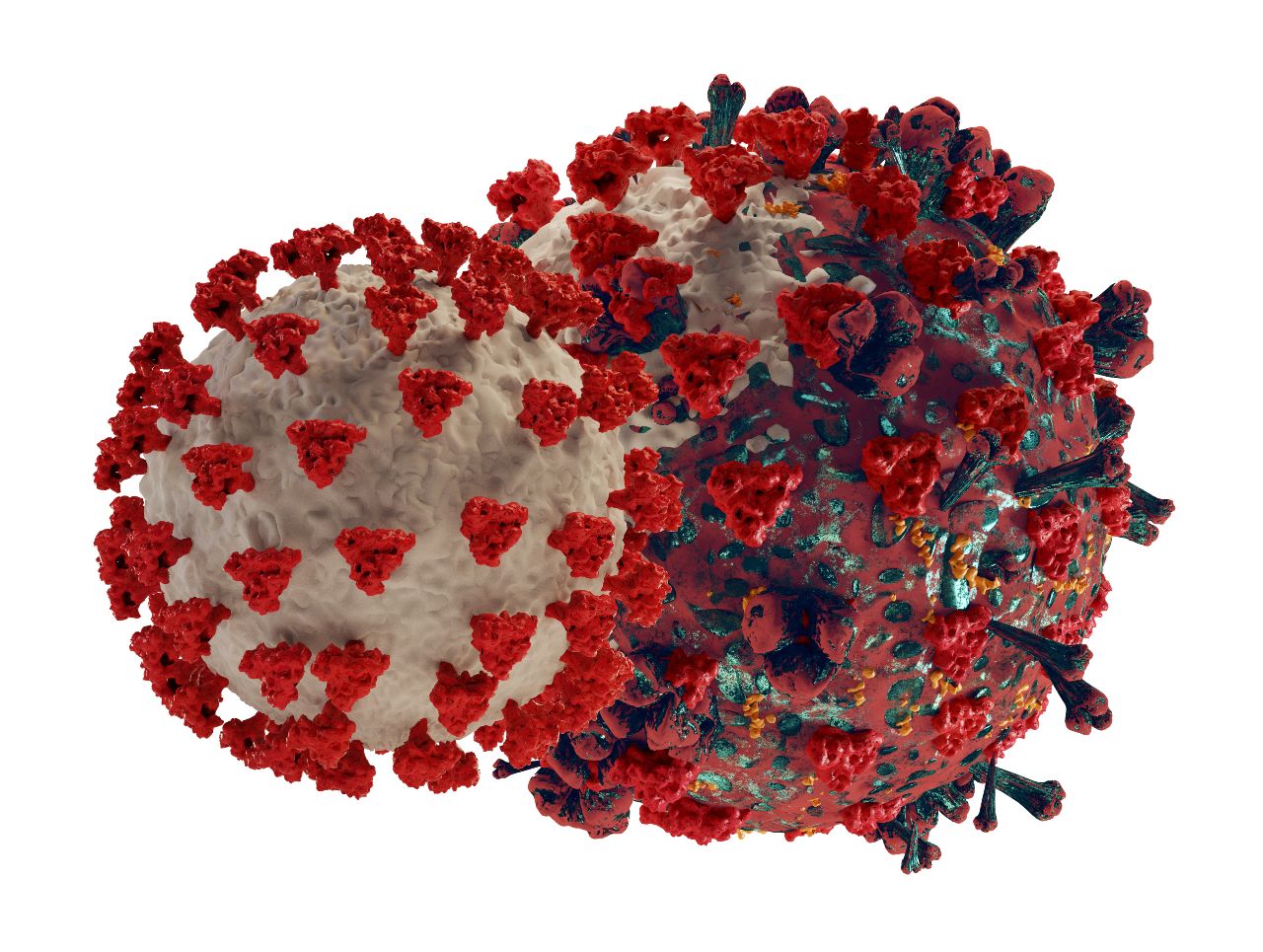
So what happens when you get infected by a virus despite being vaccinated, or the virus mutates and evades the body’s defences?
As part of the global response to Covid-19, scientists around the world have been studying the way in which the SARS-CoV-2 virus has been mutating, and seeking to discover the origin of emerging variant strains. Newly published research points to the likelihood that many SARS-CoV-2 variants are being formed in patients who already have a weakened immune system2. These patients suffer chronic and long-lasting symptoms, and because of their weakened antibody response, are unable to fully recover from the infection. This allows the virus more time to survive and replicate in the body, and results in the evolution of many new variants. If they are infectious enough, these variants then spread and can reinfect the population, causing a recurring problem like we see with the Influenza virus.
Even a virus that is thought to be all but eradicated can raise its head again and cause concern. Just last week it was reported by the UK Health Security Agency that routine testing of wastewater samples found several closely related varieties of poliovirus.3 Poliovirus is the cause of poliomyelitis (commonly called ‘polio’), a highly infectious disease that can cause limb deformities and paralysis, and which has been the target of a global eradication effort by health organisations since 1988.
The ability of viruses to mutate and evolve ways to protect themselves against the immune system means that vaccines are only a limited solution to the significant harm caused by viral disease. Antiviral drugs are another part of the arsenal.
The need for effective antivirals
Antivirals are to viruses what antibiotics are to bacteria. They can normally be prescribed after a viral infection has started, and are designed to attack the virus in some way, generally without relying directly on the immune system. However, antiviral drugs are usually highly targeted and specific to only one type of virus. They also tend to lose their effectiveness when viruses mutate. Tamiflu® is an infamous example of an antiviral drug that was initially effective but stopped working after Influenza mutated.
The first antiviral drug was approved in 1963. In the six decades since then, there have only been around 90 more antivirals formally approved, and collectively these are for the treatment of only nine viruses in total: HIV, Hepatitis B, Hepatitis C, Herpes, Influenza, CMV, Varicella-Zoster, RSV, and HPV. That leaves another 210 known human viral diseases without any approved treatment!
Kimer Med has taken on this challenge and is working on the development of a broad-spectrum antiviral. Early indications are that our compound (VTose®) will be effective against a range of viruses, and resistant to viral mutation. These are both significant factors which give us a great deal of encouragement as we continue on our quest to end viral disease.
We invite you to follow our journey and share this information to raise awareness about this important work.
References:
1.https://ourworldindata.org/covid-vaccinations?country=OWID_WRL
3. https://www.gov.uk/government/news/poliovirus-detected-in-sewage-from-north-and-east-london


